I was diagnosed Oct. 20 2002 with stage IV ovarian cancer, metastasised to my lungs. Diagnosis Day, or D-Day, as I sometimes refer to it.
I will back up from that historic (or hysteric) day to three months in July 2002 when I started having a flare up of my arthritis. I was a daily walker for an hour, a sometimes tennis player and bicycle rider, and now all my activities came to an abrupt halt. After a few visits to my family doctor for medication changes and cortisone injections, I briefly improved. I was referred to my rheumatologist after a re-occurrence and, after examination and blood work, was started on methotrexate, a drug also used as chemotherapy for cancer patients. I jokingly said, "Well, I guess I won't get cancer."
As a Registered Nurse, I knew the importance of taking care of my own health, so I always kept a log of my own health issues and doctor appointments, and yearly checkups. My yearly kitchen calendars, which I keep, also served as a reference, and I can see that I was at my family doctor and rheumatologist for complaints of leg pain, constipation, discomfort on eating, and gas, some of this attributed to the side effects of methotrexate, but also signs of ovarian cancer.
At one point, I had decided to walk through the leg pain, so I tried to begin exercising, and complained to my doctor of not having my normal stamina, which we concurred, was a result of no activity for three months. I know my lungs were then checked and no abnormalities were found. I distinctly remember that because two medical residents were also at the office that day, and I joked that they were getting practice using a stethoscope. No way do I blame any of the Doctors or myself, now knowing that ovarian cancer is called "The Whispering Disease" for a reason. There is NO test to detect it.
That was two weeks prior to D-Day, and on a Sunday morning I awoke to bloating and difficulty breathing, so immediately went to the ER.
Within two hours I was given an X-ray, EKG, blood work, ultrasound, and internal examinations, but never did I think of cancer. It was the resident gynecologist who, after reviewing tests and doing an examination, said, with her back to me, "step down from the table Mrs. McDonald, you have stage IV metastasised ovarian cancer.” I can still hear those words. Stunned is the only word that comes to mind as I stumbled out to the waiting room to get my husband, John, and, with me in a johnny shirt and bare feet, I am crying that I have cancer. Upon returning together to the exam room, I was told that I would then have my abdomen and lungs immediately drained. It was extremely scary to see so many bottles filled with bodily fluids containing cancer. Together, after somehow returning home, through the tears, the disbelief, the many breakdowns, we somehow found the strength to tell our three sons, other family and friends by numerous phone calls, and emails. I think we operated on autopilot for awhile.
Then I had three chemos, a complete hysterectomy, then three more chemos. Post surgery was complicated by an infection which resulted in a longer hospital stay. Losing my hair was one of the most traumatic experiences. I reached the magic number of below 21 on the Ca 125, a tumour marker, after five chemos, so I was reassured that chemo was working.
Although the doctors had so gently and kindly explained my chances, when I anxiously pressed for some statistics it sure was difficult to accept that I was looking at an unimpressive 20% chance to survive to five years. You can imagine the jolt when you hear this for the first time. However, after chemo #5, a doctor. said "when, not if, you come for your 5-year discharge" and this positive outlook from the medical profession went a long way in my mind.
Six years later, I was diagnosed from my yearly mammogram as having breast cancer, so this resulted in more surgery, radiation, chemo, hair loss, and 75 various appointments within a year. I always knew I was more at risk for breast cancer after the ovarian cancer diagnosis, and this was also confirmed by genetic testing.
In May 2014, again from an annual mammogram, then a follow-up CT scan, I was given the ugly diagnosis of metastatic cancer in my lungs, the other breast and a rib. Immediately, I had a procedure done on my lungs to remove the fluid and prevent more from accumulating by doing a pleuredisis, where talc is inserted into the pleural space. It was six painful days in the hospital, with a complication of an overdose on pain meds, resulting in an antidote at 3 am, and waking to see the crash cart and many staff around me. I will be closely monitored every three months, take an estrogen blocker, and continue to live as if I am living with a chronic disease.
As I reflect on what has worked for ME, I know it was many things. As I struggled to go from the caretaker role to being on the receiving end, I came (at first reluctantly), to accept all the wonderful help that was given. After my hysterectomy, a nurse gave me "hugs and drugs" in the middle of the night in the hospital, there were many phone calls, cards, visits, emails, requested jokes, tons of food when I got home, prayers from many, the visits from my church, my caring family, and much more. The best support came from my husband who immediately retired and took care of me.
I read every book I could find about stories of other cancer survivors, looking for their reason of success: used visualization of Pac-man gobbling those cancer cells; thought of the coming summer, running up that final hill to the summer cottage, then riding my beloved lawn tractor; listening to a song in my head, renaming “Hit the Road Jack,” to “Hit the Road Cancer,” then planning a trip to Las Vegas for sunshine and shows with my husband as soon as chemo was over.
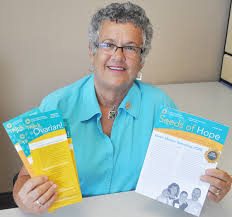
In 2002 I soon got involved with Ovarian Cancer Canada to co-chair the Walk of Hope in Halifax, did that for 6 years, served on the Board of Directors, teach well women the warning signs, and tell my story to many medical professionals so they can learn too. I have felt very blessed to have met so many courageous women with ovarian cancer, sharing a common bond through our journey. I have realized that this been the best therapy for me during the past 12 years, and now know that scientific proof of helping others improves your health. It is called “the helpers high.” Sadly, I have lost too many friends to this disease, but it makes me more determined to carry on, so I continue to do whatever I can to spread the word. I now refer to my involvement with Ovarian Cancer Canada as my "accidental passion," and it will continue as long as I live.
Just to add to my drama, in 2014, at age 69, I accidentally discovered that I was adopted. I found my “new” family with the help of a good friend. This revelation, although emotionally exhausting, proved the importance of knowing one’s genetic background, since I could have possibly escaped a late diagnosis of ovarian cancer. My biological family is filled with relatives who carry the genes, BRCA 1 and 2, and many cases of breast, ovarian and prostate cancer. So the previous adoptive family information at Genetics in Halifax had to be discarded. I thought about being a part of a study at Sunnybrook hospital, Toronto, but I felt too overwhelmed to get involved in another project. In October, my husband accompanied me to Ontario to meet two half siblings and many other “new” relatives who welcomed me into the family. My friend found the ultimate gift – a visit to the actual house where Florence had lived with another husband, and it is comforting to know that she spent 8 years is a happy environment without the poverty that she had endured. She died at 59 of heart failure.
This is now the beginning of 2016, and I have recently been told that the current chemo is no longer working, and I possibly have only months to live. That would fill a book, but I am extremely grateful to all the friends, family and newcomers who put the puzzle together, giving me peace.
Thanks to all of you for reading my story, and good health to all…
 RSS Feed
RSS Feed